Coccygeus muscle
| Coccygeus muscle | |
|---|---|
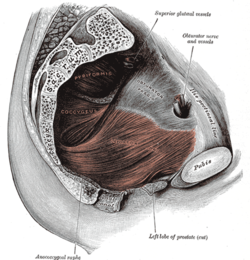 Left levator ani from within. | |
| Details | |
| Origin | Sacrospinous ligament and ischial spine |
| Insertion | Lateral margin of coccyx and related border of sacrum |
| Nerve | Pudendal nerve; sacral nerves: S4, S5[1] or S3-S4[2] |
| Actions | Pulls coccyx forward after defecation, closing in the back part of the outlet of the pelvis |
| Identifiers | |
| Latin | musculus coccygeus |
| TA98 | A04.5.04.011 |
| TA2 | 2412 |
| FMA | 19088 |
| Anatomical terms of muscle | |
The coccygeus muscle or ischiococcygeus is a muscle of the pelvic floor located posterior to levator ani and anterior to the sacrospinous ligament.
Structure
[edit]The coccygeus muscle is posterior to levator ani and anterior to the sacrospinous ligament in the pelvic floor. It is a triangular plane of muscular and tendinous fibers. It arises by its apex from the spine of the ischium and sacrospinous ligament.[3][4] It is inserted by its base into the margin of the coccyx and into the side of the lowest piece of the sacrum.[3][4]
In combination with the levator ani, it forms the pelvic diaphragm.[5]
The pudendal nerve runs between the coccygeus muscle and the piriformis muscle, superficial to the coccygeus muscle.[6]
Nerve supply
[edit]The coccygeus muscle is innervated by the pudendal nerve, which runs between it and the piriformis muscle.[7]
Function
[edit]The coccygeus muscle assists the levator ani and piriformis muscle in closing in the back part of the outlet of the pelvis.[8] This helps to support the vagina in women, and the other pelvic organs.[8]
See also
[edit]References
[edit]![]() This article incorporates text in the public domain from page 424 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 424 of the 20th edition of Gray's Anatomy (1918)
- ^ Essential Clinical Anatomy. K.L. Moore & A.M. Agur. Lippincott, 2 ed. 2002. Page 217
- ^ "uams.edu". Archived from the original on 2007-12-16. Retrieved 2007-12-09.
- ^ a b Ho, MAT H.; Bhatia, NARENDER N. (2007-01-01), Lobo, Rogerio A. (ed.), "CHAPTER 51 - Lower Urinary Tract Disorders in Postmenopausal Women", Treatment of the Postmenopausal Woman (Third Edition), St. Louis: Academic Press, pp. 693–737, doi:10.1016/b978-012369443-0/50063-6, ISBN 978-0-12-369443-0, retrieved 2021-02-07
- ^ a b Sokol, Andrew I.; Walters, Mark D. (2007-01-01), Sokol, Andrew I.; Sokol, Eric R. (eds.), "Chapter 23 - Pelvic Organ Prolapse and Pelvic Floor Dysfunction", General Gynecology, Philadelphia: Mosby, pp. 543–581, doi:10.1016/b978-032303247-6.10023-1, ISBN 978-0-323-03247-6, retrieved 2021-02-07
- ^ Barone, William R.; Abramowitch, Steven D.; Moalli, Pamela A. (2015-01-01), Badylak, Stephen F. (ed.), "Chapter 13 - Host Response to Biomaterials for Pelvic Floor Reconstruction", Host Response to Biomaterials, Oxford: Academic Press, pp. 375–423, doi:10.1016/b978-0-12-800196-7.00013-x, ISBN 978-0-12-800196-7, retrieved 2021-02-07
- ^ Bennett, Richard C.; Peters, Kenneth M. (2008-01-01), Raz, Shlomo; Rodríguez, Larissa V. (eds.), "Chapter 24 - PUDENDAL NERVE STIMULATION", Female Urology (Third Edition), Philadelphia: W.B. Saunders, pp. 284–289, doi:10.1016/b978-1-4160-2339-5.50073-2, ISBN 978-1-4160-2339-5
- ^ H. Kim, Daniel; A. Murovic, Judith (2008-01-01), Kim, Daniel H.; Midha, Rajiv; Murovic, Judith A.; Spinner, Robert J. (eds.), "11 - Lower extremity nerve injuries", Kline and Hudson's Nerve Injuries (Second Edition), Edinburgh: W.B. Saunders, pp. 209–278, doi:10.1016/b978-0-7216-9537-2.50019-0, ISBN 978-0-7216-9537-2, retrieved 2021-02-07
- ^ a b Muir, Tristi W. (2008-01-01), Raz, Shlomo; Rodríguez, Larissa V. (eds.), "Chapter 74 - POSTERIOR WALL PROLAPSE: SEGMENTAL DEFECT REPAIR", Female Urology (Third Edition), Philadelphia: W.B. Saunders, pp. 729–736, doi:10.1016/b978-1-4160-2339-5.50123-3, ISBN 978-1-4160-2339-5, retrieved 2021-02-07
External links
[edit]- Anatomy photo:43:16-0103 at the SUNY Downstate Medical Center - "The Female Pelvis: Muscles of the Pelvic Diaphragm"
- Cross section image: pelvis/pelvis-e12-15—Plastination Laboratory at the Medical University of Vienna
- pelvis at The Anatomy Lesson by Wesley Norman (Georgetown University) (femalepelvicdiaphragm, malepelvicdiaphragm)
- Coccyx pain, tailbone pain, coccydynia (Peer-reviewed medical chapter, available free online at eMedicine)
